Achieving operational economy through facility design is the central focus of designing for efficiency in healthcare facilities. The economies can impact building size and shape as well as staff savings. The staff savings are sometimes related to helping nurses spend more time at a patient’s bed side as well as opportunities to reduce the total number of staff needed to operate a hospital.
Opportunities to reduce the number of staff needed can have a substantial impact, especially in markets where there are shortages of qualified personnel. Designing for efficient facilities begins at the master site plan and continues through details relating to horizontal and vertical transportation on all floors of a facility, including the size and shape of departments and continues to establishing the location of supplies on the individual patient care areas.
Facility Master Plan
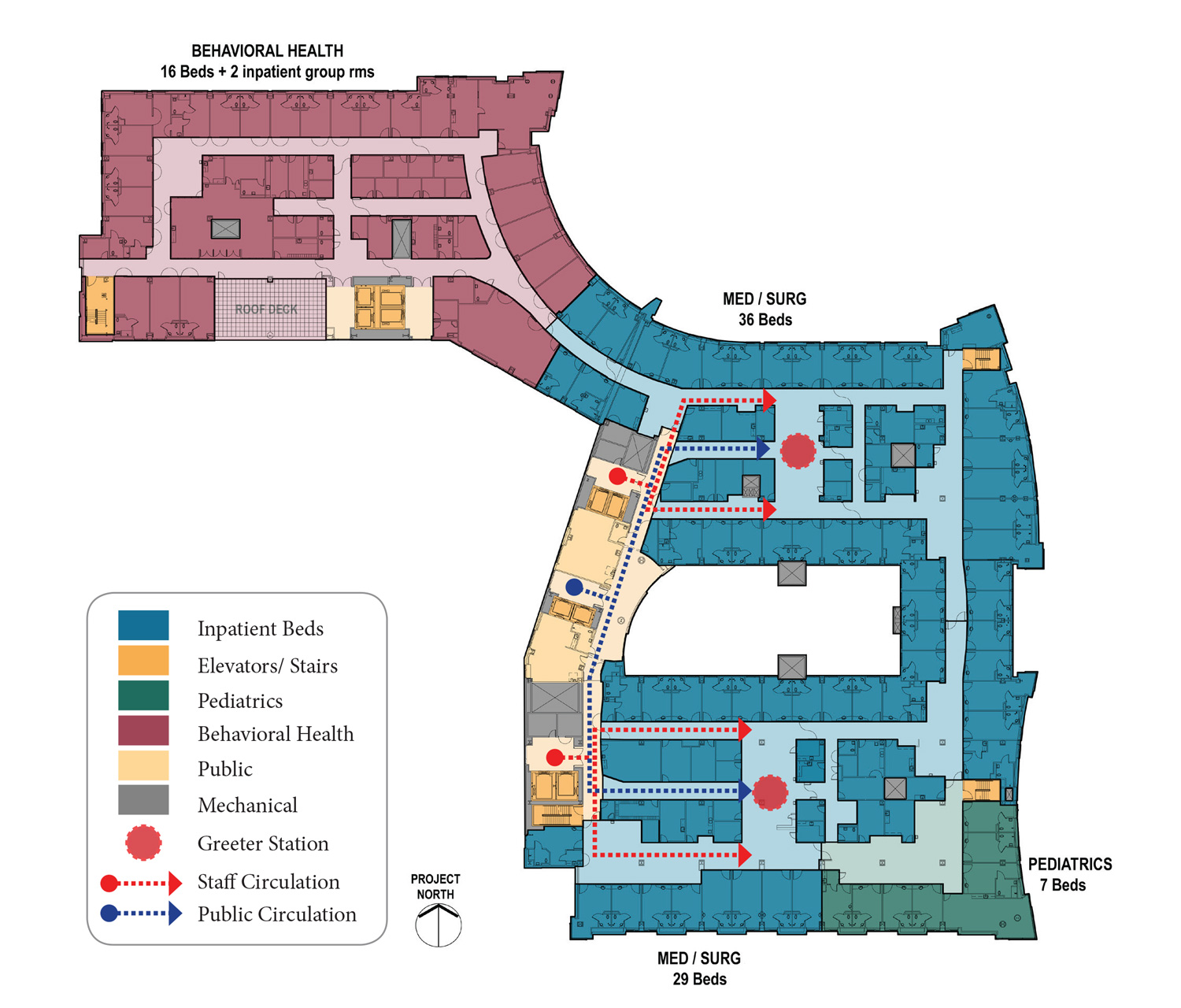
Circulation Diagram
SITE ORGANIZATION & TRAFFIC FLOW
Providing a clear organization to the site is central to the creation of an efficient operational model. Therefore, early site selection is important in providing optimum conditions for the different types of access and traffic flow – ideally a location with a minimum of two access streets. Also, a site’s size can be a determining factor for a hospital’s projected capacity and future growth as well as having an impact on operational efficiency. Once chosen, the site is the first opportunity to establish a hierarchy of circulation with separate movement for public traffic, emergency traffic and support / service traffic and occasionally a separate traffic pattern for staff.
The concept of on-stage and off-stage is consistent with this hierarchy although the number of traffic routes at a hospital is more complex at the site level with three to four patterns to differentiate. The premise of on-stage and off- stage movement is to allow the off-stage support operations to function with fewer interruptions, more efficiently. The same premise dictates a need to allow emergency vehicles to access the hospital with the least chance of interaction with the public and support / service traffic. Avoiding conflicts in traffic flow should allow for the greatest degree of efficiency as well as not delaying an ambulance arriving at the emergency department because it was blocked by a delivery vehicle maneuvering into the loading dock.
BUILDING SHAPE & SIZE
The geometry of the buildings can have an impact on the efficiency of the internal spaces. Irregular building shapes often result in less efficient plans and may result in extra or less usable space. This should not be construed to mean that only a simple rectangular shape is always the more efficient. It is important to understand and to consider alternative shapes as well as the functions that will be taking place inside the hospital building, or a portion of a hospital building, as well as future flexibility to connect or grow a particular portion of the hospital.
The building shapes impact the efficiency of internal spaces.
Large uniform and very regular rectangular blocks of space are ideal for an efficient layout for large diagnostic and treatment services such as Surgery, Radiology and Emergency. However, these simple large boxes are typically not as ideal for an efficient inpatient bed unit. Because different shapes are more efficient for different internal functions, many healthcare facilities reflect these differences at the site plan level. The differences are not always apparent at the site plan due to site restrictions such as site size and zoning setbacks, so that the ideal shapes for an inpatient care unit may not be apparent until the upper floors of a hospital.
Building & Departmental Organization for Efficiency
500 Bed Hospital Prototype Medical-Surgical Unit
BUILDING ORGANIZATION
Where are the elevators? No other element of the hospital building has a greater impact on the efficiency of the facility than the placement of vertical transportation, the elevators and occasionally in very large facilities, escalators. On-stage and Off-stage circulation are critical in the placement of the vertical transportation to ensure that supplies move efficiently to the care areas, as well as providing discrete routes so that patients can be transported without mixing with the public. Relationships between the loading docks, materials handling, food services and the elevators are the drivers at the service floor level while the distance from the elevators to supply and distribution facilities in the care areas are the drivers on the patient care or treatment floors. The need to reduce horizontal travel at each end of the circuit from the delivery to the facility to delivery of care is paramount for the efficient operation of the hospital.
How materials are moved into the patient care areas are important to understand for an efficient flow. Providing a route for materials / supplies / food carts to enter units away from the public route is ideal for maintaining a smooth flow, while also enhancing the public’s experience in the hospital. Similar separations are important in the diagnostic and treatment facilities to allow the public / outpatients to enter and move through the department with minimal interaction with the flow of support services, the supply / delivery functions and the removal of waste.
Theories regarding the separation of supplies from patients and waste stream from supply stream are numerous. In some regions, the separation of the supply and waste streams is mandated by code. However, in other regions the movement of the supplies and the waste has been merged into common more efficient circulation patterns reducing redundant circulation. In these cases, the movement of waste as well as the movement of supplies is within closed containers. The redundant clean and soiled circulation has not been proven to reduce infections, further justifying the merged circulation. In addition, the operational cost of the closed containers is far less than the construction cost of the redundant circulation and the extra time and often dedicated staff needed to move the separated supply and waste stream materials in their discrete corridor and elevators.
Reducing trips on elevators, such as through the use of linen and trash chutes, can facilitate efficiencies both on the patient care unit as well as at the service floor.
El Camino Hospital, Mountain View, CA | Nursing Floor Plan
STANDARDIZED BUILDING ELEMENTS & UNIT CONFIGURATIONS
The use of standardized building elements, such as a standard exam room or a standard inpatient bed room, can simplify and reduce construction schedules as well as positively impact repairs and replacement by reducing the variations in the elements that need to be repaired or replaced. The standardization of building elements can also provide efficiencies in the operation of departments. For example, using a standardized exam room in the Emergency Department with mobile carts for specialty support, such as orthopedic casting, allows greater flexibility in the scheduling of the exam rooms, with no dedicated rooms sitting idle for long periods.
MD Anderson Cancer Center Ambulatory Hospital, Houston, TX
The greater flexibility in scheduling provides greater efficiency to more fully utilize all of the exam rooms and in the initial construction can lead to a smaller number of exam rooms that are needed. In another example, by standardizing the exam rooms in a clinic, not only can similar scheduling and utilization efficiencies occur, but if one clinic needs more clinic exam rooms on some days and another clinic needs fewer, the clinics can flex into the adjoining clinic—utilizing any underused capacity. Again, the result is a more efficient utilization of the resources and can lead to the need to initially build fewer clinic exam rooms.
MD Anderson Cancer Center, Houston, TX | Floor Plans for Ambulatory Services
To allow for the greatest efficiency from the repetition of these standardized building elements, the configuration of the standardized elements must follow a formal discipline so that the groups of exam or other rooms support the efficient scheduling and shifting of volume. Repetitive modules or groups of standardized building elements with standardized support allow for the greatest degree of efficiency.
The module for a typical clinic floor is planned for zones of exam rooms, work areas and public circulation as shown here for the MD Anderson Cancer Center.
MERGING OF OR CO-LOCATION OF SIMILAR SERVICES
Perhaps one of the avenues for creating the greatest first cost and long term operational cost savings is the merging or co-location of similar services. Examples include the co- location of surgery and other procedure services, including endoscopy and cardiac catheterization, into a single Interventional Platform as well as merging both inpatient and outpatient imaging departments.
The creation of the Interventional Platform provides an opportunity to merge all of the preparation and recovery functions for these procedure services. The savings that are possible include significant staff savings resulting from having a single versus sometimes three separate prep & recovery areas as well as a reduction in the total number of prep and recovery positions that need to be constructed and the number of utility / service rooms needed to support the separate prep and recovery areas.
While many hospitals have merged inpatient and outpatient diagnostic imaging departments, the concept of providing separate departments is often considered. The reason for this consideration is most commonly focused on keeping inpatients far removed from outpatients. However, the operational efficiencies of a merged department can be substantial. In one case study, the merged department required as many as three fewer imaging rooms and more than five fewer FTE’s to operate the merged department compared to the two departments.
El Camino Hospital | Level 2
STAFF EFFICIENCY IN THE PATIENT UNIT
Extensive evidence based research has been conducted over recent years focusing on the most efficient arrangement of spaces on inpatient bed units. Some of the research has re-introduced an approach to supplies that was previously abandoned. The decentralization of supplies close to or inside a patient room was previously abandoned as an inefficient utilization of staff and space resources.
However, recent studies emphasizing the need to allow nurses to spend more time with the patients and less time retrieving supplies has reversed the approach. There has been a trade-off between a less efficient supply staff process of loading one or two large supply rooms to a more efficient nurse distribution to the patient process, which requires the supplies to be initially stocked to multiple locations, typically inside the patient room.
Another driver for abandoning the distributed system previously was greater inventory control in the central supply rooms. With improved computer inventory systems, this reason for centralized supplies is no longer an issue. Some research has shown that the minor increase in space associated with the patient rooms is justified by the more efficient utilization of the nursing staff.
Even with supplies and often patient specific medications distributed to the patient room, the shape, size and configuration of the patient unit remain critical factors for the design of an efficient patient unit. It is still desirable to minimize the distance that staff needs to travel between the main support rooms, including the central staff work areas, and the patient rooms. The efficient movement of supplies, waste and the patient needs to be considered as various geometries are tested for the patient unit.
In addition, the configuration of the patient rooms can have an impact on the efficiency of the unit. Standardized rooms that are square or wider than they are deep, such as rooms with nested toilets, can add significant travel distances to the units and will greatly reduce the efficiency of supplying the beds, removing waste from the beds and moving the patients. Rooms that are deeper between the corridor and the exterior wall tend to support a more efficient model.
Medical Surgical Unit
Summary
Efficient design is central to healthcare facilities. It drives how the facilities are placed on the site as well as the shape of the buildings. As the design for the healthcare facility is developed at the departmental level, efficiency is often the primary reason behind most decisions. And most important, an efficiently designed hospital can cost less to build and operate as well as requiring fewer staff.
For more information contact Nick Putnam